Recognizing BBS
The importance of early diagnosis for people living with BBS
People with early-onset obesity due to BBS are at risk of long-term health complications1
Identifying the type of obesity in your patient can:
- Help you determine the optimal management of their specific disease2
- Reduce the cumulative impact of their obesity, especially if diagnosed early1,3
- Bring a sense of relief to patients4
People living with Bardet-Biedl syndrome (BBS) and their families often gain a sense of relief in knowing there is an underlying cause of their symptoms unrelated to environmental and lifestyle factors.
Early identification allows patients and families to plan, prepare, and better manage their disease.2.5
Diagnosing BBS
BBS is a ciliopathy with a highly variable phenotype and clinical features that vary greatly across individuals and evolve over time. Some features may present more mildly or slowly depending on gene variant and other factors.2,6–9

Recognizing BBS in Children
- Due to the progressive onset of clinical symptoms, patients may not meet the diagnostic criteria early in life, leading to a potential delay in diagnosis10
- Therefore, genetic testing may play a critical diagnostic role in young children10
Diagnosing patients as early as possible is key to reducing their weight gain trajectory and managing associated obesity outcomes. It may also help reduce the burden of hyperphagia.10

Recognizing BBS in Adults
Many people over 30 with BBS may not have been diagnosed as children due to the following limitations11,12:
- Clinical diagnosis: Clinical diagnosis criteria were newly defined when they were children. Clinical recognition of the syndrome also remains low due to variability in phenotypical presentation10
- Genetic confirmation: In 1999, only 4 of the current BBS genes had been identified. Also, there has been historically low genetic-testing utilization due to a lack of availability, insurance coverage, and treatment for BBS9,11
It is important to recognize the symptoms of BBS in adults to ensure they are diagnosed appropriately.
Downloadable
Identify hyperphagia and early-onset obesity given the risk of potential long-term complications. Utilize this diagnosis guide for an in-depth understanding of BBS.
Genetic testing can be integrated into the overall clinical assessment of the patient and does not equate to a diagnosis on its own.
Additionally, variant interpretation may change over time as the information about the genetics of BBS continues to evolve.
Genetic testing through the Uncovering Rare Obesity® program is available for eligible patients.
Get connected. Find resources and get more information.
Managing obesity and hyperphagia due to BBS
Patients may experience short-term weight loss with some interventions, but these approaches have shown limited efficacy in producing sustained results as they do not address the underlying pathophysiology.7,12,13
Diet & Behavior Modifications14,15
Diet and exercise may have little impact for people living with a rare genetic disease that causes obesity, like BBS
Pharmacotherapies2,16
The goal of treatment for obesity due to BBS should be individualized and tailored to each patient and address the underlying cause
Bariatric Surgery14,17
There is a lack of robust, long-term efficacy of bariatric surgery in people living with BBS. Significantly, they may not be considered suitable candidates due to common features such as hyperphagia or cognitive impairment
Find out about a treatment option for obesity due to BBS.
Support for BBS
Patients living with BBS may not understand the full impact of their disease, so informational resources and one-on-one education can make a meaningful difference.
BBS Resources
Diagnosis Guide
Notice the signs and symptoms of BBS
Ophthalmologist Guide to BBS
An ophthalmologist may be the first doctor a patient with BBS sees for care
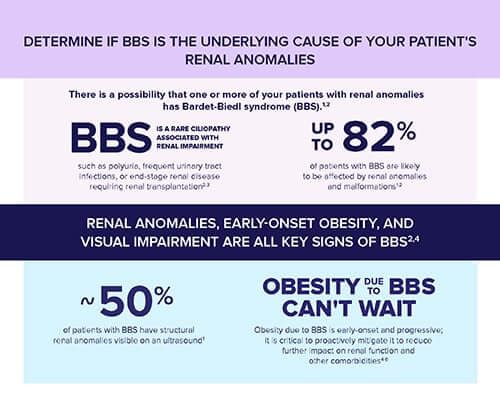
Nephrologist Guide to BBS
A nephrologist may play an important role for patients with BBS
BBS Rhythm InTune Patient Education Handout
Share this handout with patients to inform them about personalized one-on-one educational support
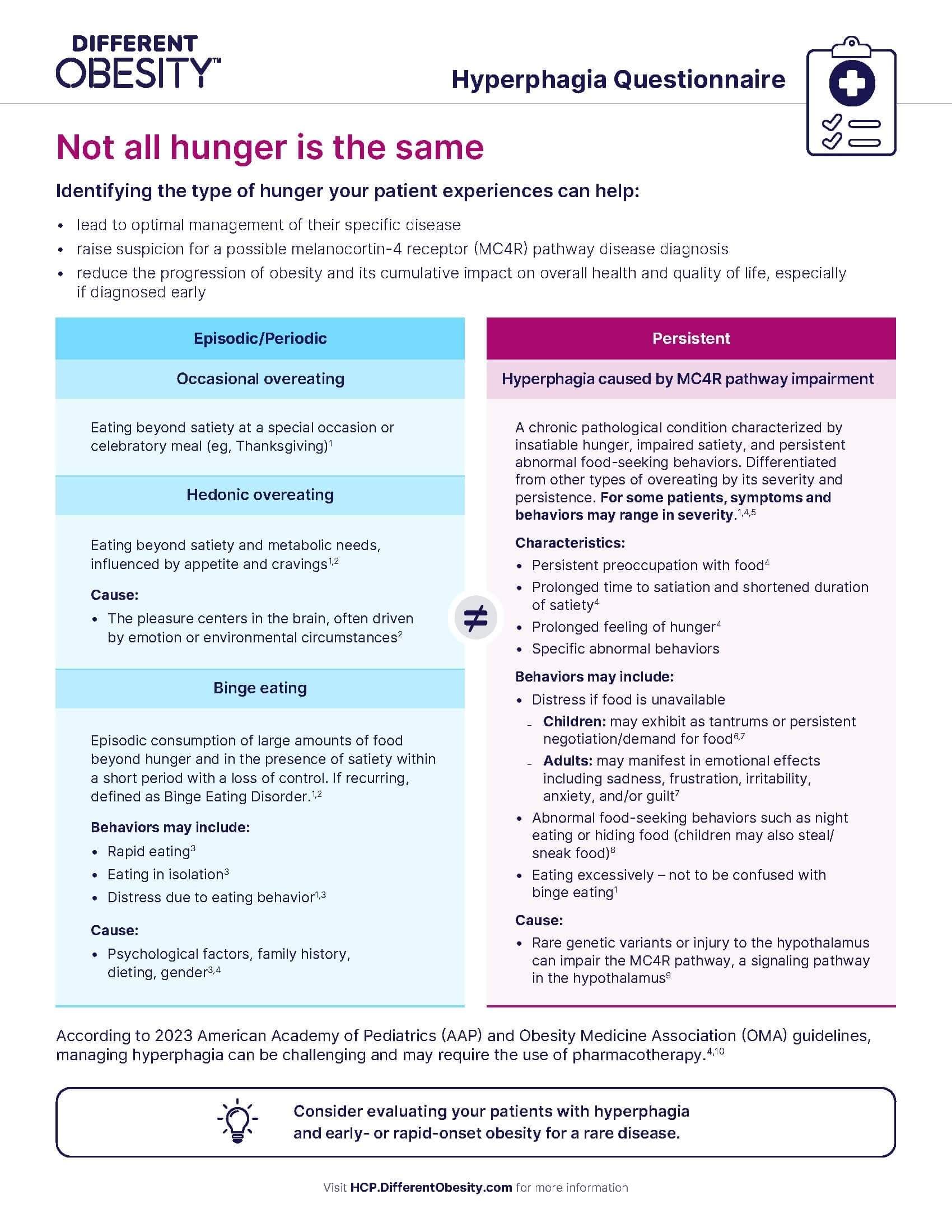
Hyperphagia Questionnaire
Identify hyperphagia in your patients with BBS
Join the HCP Directory
Be included in our list of healthcare providers who manage patients with rare diseases that cause obesity

MC4R pathway video Watch the role of the MC4R pathway in BBS

Amy and Alex’s Story View Amy and her children’s life with BBS

Olivia, Adalissa, and Solomon’s Story Hear from Olivia, a mother to Adalissa and Solomon who are living with BBS

Leigh and Izzy’s Story Watch Leigh and Izzy’s story of what living with BBS is like
Sign up to receive educational resources for your patients and practice, as well as updates about BBS.

Personalized one-on-one educational support* for your patients living with BBS
Rhythm InTune provides educational resources, wellness tips, and connection to a community for people living with BBS
Patient Education Managers are employees of Rhythm Pharmaceuticals and do not provide medical care or advice. We encourage patients to always speak to their healthcare providers regarding their medical care.