Bardet-Biedl Syndrome
BBS overview
Actor portrayal
BBS ciliary dysfunction impairs various systems throughout the body1,2
Bardet-Biedl syndrome (BBS) is a rare autosomal recessive ciliopathy that is clinically and genetically diverse.3
Two key features among a wide range of symptoms
Hyperphagia and obesity are among the common features of BBS that can seriously impact the overall health and quality of life of these patients.3,4
Hyperphagia5–7
Chronic pathological condition characterized by insatiable hunger, impaired satiety, and persistent abnormal food-seeking behaviors.
Early-onset obesity5,8–12
Early onset obesity may develop as early as 2 years old, often appearing in early childhood and continuing into adolescence and adulthood.
Signs and symptoms of BBS
Primary cilia dysfunction within each organ system contributes to the highly variable phenotype in BBS, which evolves significantly during childhood and into adolescence.3,13
Brain3,5
- Hyperphagia
- Early-onset obesity 72-92%
- Cognitive impairment 61%
Kidneys3,14
- Renal anomalies 53-82%
Reproductive3,15
- Hypogonadism 59-98%
Eyes3,16
- Rod-cone dystrophy/retinitis pigmentosa 93%
Skeletal3
- Polydactyly 63-81%
Additional clinical features of BBS may include3,9:
- Brain: speech delay, developmental delay, ataxia/poor coordination, anosmia/hyposmia
- Endocrine: diabetes mellitus
- Heart: congenital heart disease
- Skeletal: dental anomalies, brachydactyly, syndactyly
People living with BBS and their families often gain a sense of relief in knowing there is an underlying cause of their symptoms unrelated to environmental and lifestyle factors. Early identification allows patients and families to plan, prepare, and better manage their disease.4,5

“It’s a constant need to eat. And that’s when she started sneaking foods... We ended up getting some locks and putting them on our pantry and on the fridge.
– Caregiver of an individual living with BBS
Causes of BBS
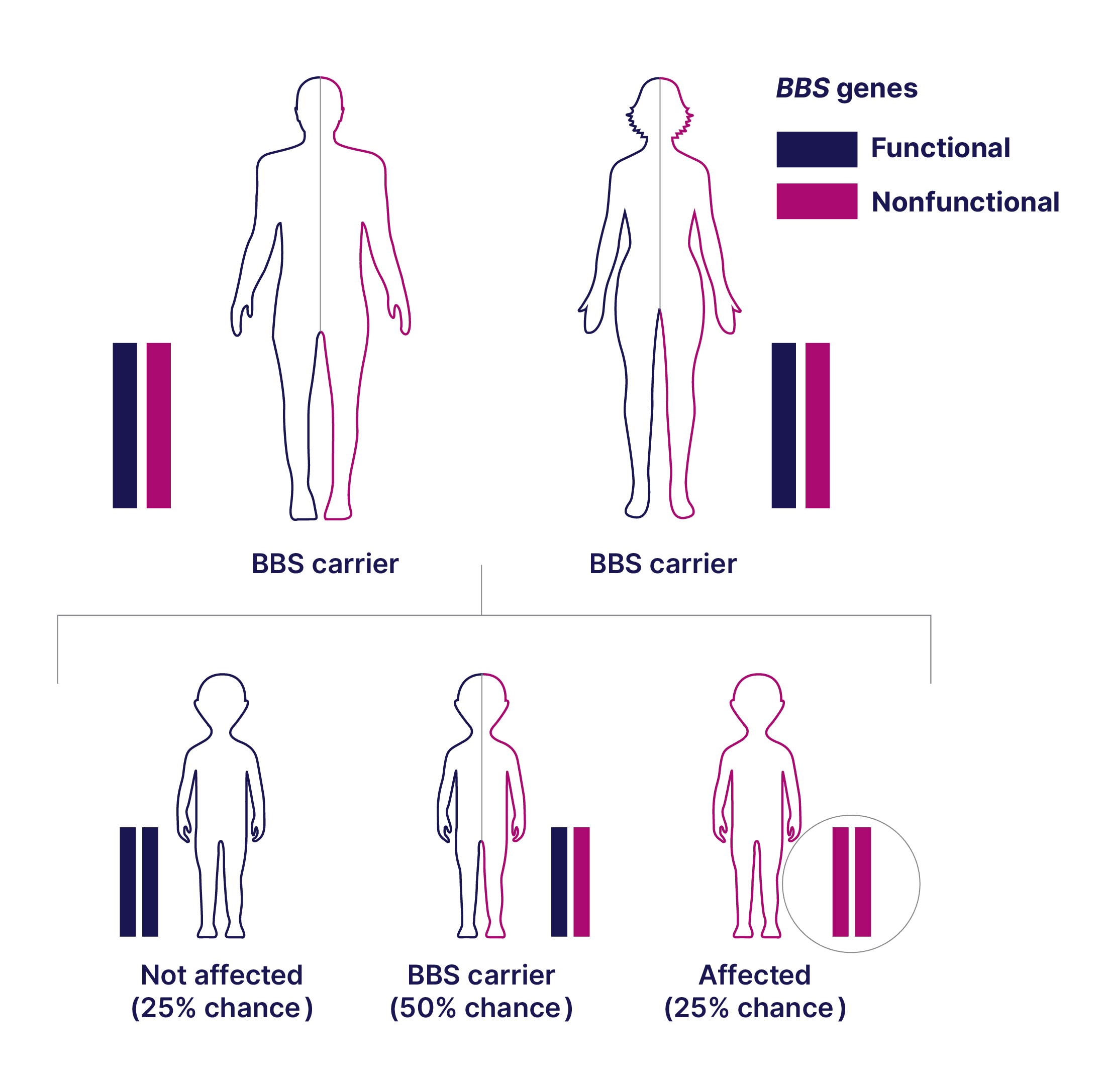
Typical mode of inheritance17-19
Affected individuals have a variant in both copies of a BBS gene. Nearly 30 genes have been found to be associated with BBS.17,18
Genetic testing for BBS can provide additional diagnostic information to help inform your diagnosis.
Results should be integrated into the overall clinical assessment of the patient and do not equate to a diagnosis on their own. Additionally, variant interpretation may change over time as the information about the genetics of BBS continues to evolve.
Genetic inheritance of BBS17,19
BBS is inherited in an autosomal recessive manner:
- Affected individuals have a variant in both copies of a BBS gene (biallelic genotype, which can be homozygous or compound heterozygous)
- Both parents of the affected individual are likely carriers of a single variant
- Not typically observed in every generation
Biallelic Genotypes
Homozygous
Compound
Heterozygous
Genetic testing may help reveal disease-causing genetic variants. The American College of Medical Genetics and Genomics (ACMG) classifies variants into 5 categories20:
Pathogenic
Likely Pathogenic
Variant of Uncertain Significance (VUS)
Likely Benign*
Benign*
Genetic testing through the Uncovering Rare Obesity® program is available for eligible patients.
Mechanism of disease
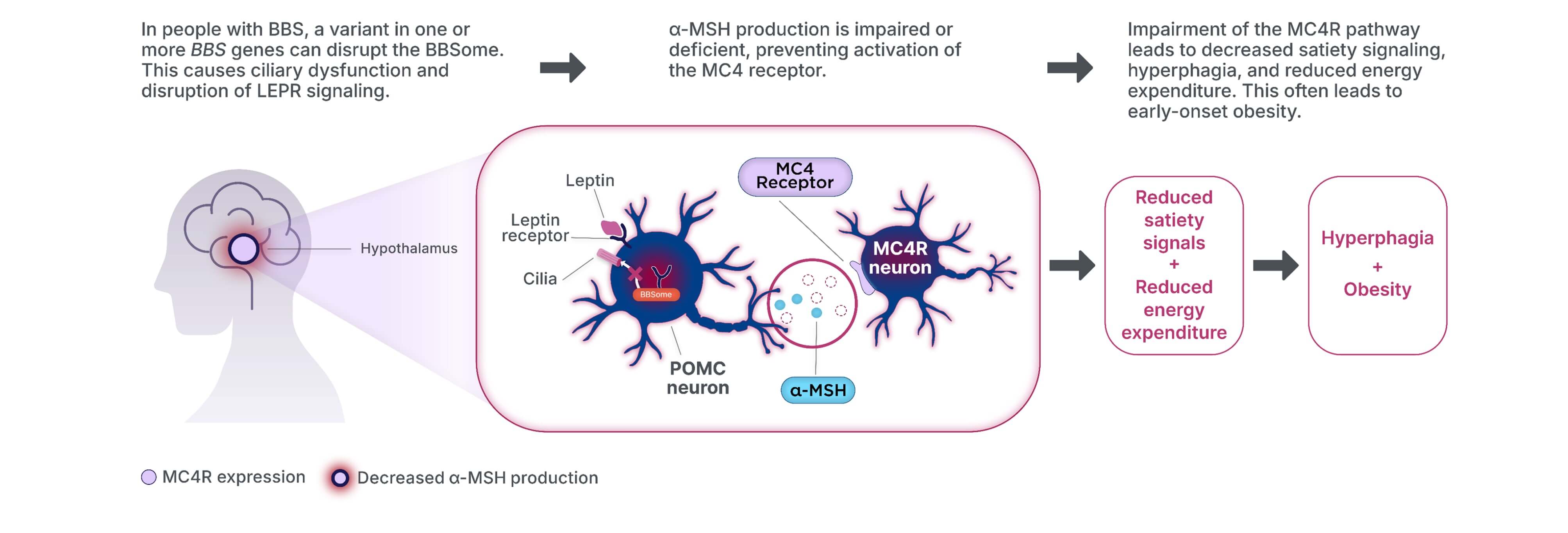
Ciliary dysfunction in BBS can lead to impairment of the melanocortin-4 receptor (MC4R) pathway—an underlying cause of obesity in BBS—setting it apart from general obesity.1–3,13
The MC4R pathway regulates hunger, satiety, and energy expenditure.1,5,21
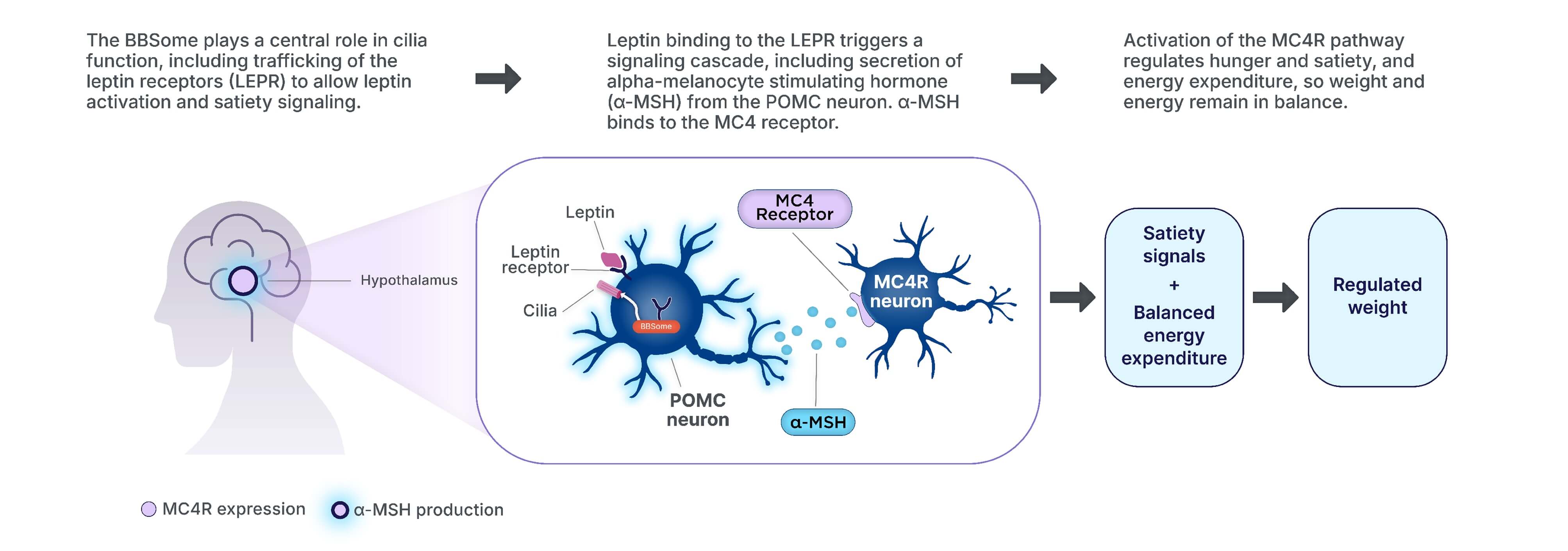
Loss of BBS gene function can impair MC4R pathway signaling, ultimately
leading to hyperphagia and early-onset obesity.1,5,22
POMC=Proopiomelanocortin
Take a deeper look inside the MC4R pathway
See the role of the MC4R pathway in driving obesity and hyperphagia in people living with BBS.

MC4R pathway video